L-PRF Perio2000 Videos
Emeritus Professor Marc Quirynen
Preparation of L-PRF clot, membrane, plug, exudate
Collect blood, utilizing special tubes which promote the coagulation. Rotate tubes immediately after blood draw to increase the contact between inner tube surface and blood. Place the first 2 tubes of blood immediately after collection in the centrifuge, opposite to each other, and start the centrifugation. Collect the 3rd and 4th tube of blood, stop centrifuge and add the new tubes to the centrifuge. Repeat this procedure for the remaining tubes. After centrifugation, collect all tubes and remove the L-PRF (fibrin) clots from the tubes, and carefully separate them from the red blood cells. Do not cut the remaining red (face) portion of the clot away; this is the most biologically active part. Compress clots gently (by gravity), using the light metal plate and cover of compression box, to form L-PRF membranes (5 min). The liquid leaking out the clots is called the exudate. Plugs can be prepared via the white cylinders.
Preparation of L-PRF bone-block, liquid fibrinogen
Collect 6 blood tubes for L-PRF membranes (see previous video), and 2 "inert" blood tubes for liquid fibrinogen (the latter only requires 3 min of centrifugation; after which you need to aspirate immediately the yellow liquid up to the red blood cell layer). Prepare L-PRF membranes. Chop 2 membranes into very small pieces (± 2-3 mm). Combine the chopped membranes and bone substitute in a small dish in a ratio of 2 membranes to 0,5 g biomaterial (corresponding to a volume of roughly 50/50), ensuring a homogenous mixture. Spray the liquid fibrinogen abundantly over the mixture and stir gently for approximately 15 seconds to bring the liquid fibrinogen in contact with the entire mixture. The fibrinogen will immediately start to clot into a 3D fibrin network, which will trap the biomaterial to form the L-PRF bone-block. Liquid fibrinogen will spontaneously coagulate after about 30 minutes; timing is crucial. The mixture can be shaped into the desired form within approximately 1 minute, after which it will hold its shape.
Alveolar ridge preservation: nearly intact socket

Start with an a-traumatic extraction and remove all pocket epithelium and granulation tissue. Rinse socket with L-PRF exudate (= antibacterial). Prepare envelope (between the bony borders of the socket and the periosteum). Tightly pack several L-PRF plugs/membranes in the socket (optimal condensation is crucial). Seal the entrance to the socket with two layers of L-PRF membranes. Slide these membranes in the envelope created between periosteum and bony socket borders, covering 3 to 5 mm of bone. Suturing is completed without any attempt to close the wound; its only purpose is to keep the L-PRF in the socket (healing by secondary intention, no flap). Small perforations in the socket walls can improve the vascularisation, and as such the healing & bone formation.
Alveolar ridge preservation: nearly intact extraction socket: details

Start with an a-traumatic extraction (consider root separation). Remove all pocket epithelium and granulation tissue (bur). Preserve inter-radicular bony septa. Prepare envelope (between the bony borders of the socket and the periosteum). Tightly pack several L-PRF plugs in the socket (optimal condensation). Seal the entrance to the socket with two layers of L-PRF membranes. Slide these membranes in the envelope created between periosteum and bony socket borders, covering 3 to 5 mm of bone. Suturing is completed without any attempt to close the wound; its only purpose is to keep the L-PRF in the socket (healing by secondary intention). Small perforations in the socket walls can improve the vascularisation, and optimise the healing.
Alveolar ridge preservation: major bony dehiscence (L-PRF only)

A buccal bony dehiscence has to be covered first, by at least a double layer of
L-PRF membranes (extending 5 mm beyond its bony borders). The face portion of the inner L-PRF membrane should preferably be facing the bony dehiscence. L-PRF membranes are tightly packed into the socket and into the bony dehiscence. The entrance to the socket is sealed with a double layer of L-PRF membranes. Suturing is completed without any attempt to close the wound, its only purpose is to keep the L-PRF in the socket (healing by secondary intention). Deeper sutures should not run over the bony dehiscence because it might push the L-PRF out of the socket; sutures must be supported by bone. Small perforations in the socket walls can improve the vascularisation, and as such optimise the healing and bone formation.
Transcrestal sinus floor augmentation (L-PRF only)
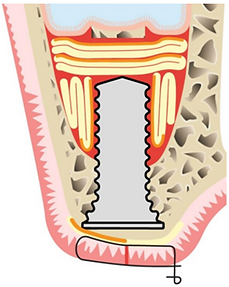
After preparing the osteotomy, up to 1 mm distance from the floor of the sinus, the last mm can be fractured with an osteotome (use an L-PRF membrane as cushion), or removed with another technique (e.g., piezo device, osseo-densification burs). At this stage, several membranes have to be inserted into the sinus via the osteotomy (with an osteotome), to lift the Schneiderian membrane. In total 4 to 5 membranes are required for a single implant in order to gain enough bone height. At the end the implant can be placed, and its cover-screw can be covered with an L-PRF membrane to speed-up the soft-tissue healing.
One-stage sinus floor augmentation (window) with L-PRF membranes & implant

Prepare a lateral window (either use the bony window to cover the entrance to the sinus at the end of the surgery, or push it inside to serve as a new floor for the sinus). The latter supports the formation of bone over the implant apex, but increases the risk for a sinus membrane perforation. Meticulously elevate the Schneiderian membrane and prepare the osteotomy (eventually protect sinus membrane with L-PRF membranes). Fill the created space with L-PRF membranes, and insert the implant. Add additional membranes around the implant and fill the window with L-PRF membranes. Seal the entrance to the sinus with another L-PRF membrane.
Two-stage sinus floor augmentation (window) with L-PRF bone-block

When a simultaneous implant placement is impossible, one can use an L-PRF bone-block (a combination of a bone substitute, liquid fibrinogen, and small pieces of an L-PRF membrane). Most steps are similar to those in previous video. After elevation of the Schneiderian membrane, the created space can be filled with parts of the L-PRF bone-block. Afterwards, the sinus window can be filled with an L-PRF membrane, and the entrance to the sinus can be sealed with another L-PRF membrane (face portion towards the sinus). Perforations in the alveolar bone (eventually through and through) will increase, if needed, the blood supply to the graft, and can optimise the bone formation. The implant can be installed after 4-6 months.
Horizontal bone augmentation: "simultaneous" approach with an L-PRF bone-block

Reflect a full thickness flap and remove remnants of periosteum or granulation tissue. Prepare osteotomy for the implant and small perforations in the receptor bone to guarantee an optimal blood supply and a strong connection between graft and native bone. Insert implant and fix an absorbing membrane apically at the buccal site. Apply the L-PRF bone-block and fix the membrane on the palatal site. Immobilise the flap (coronal advancement) to achieve tension free closure. Suture for a healing by primary intention.
So far it is not well understood whether a slow-absorbing or non-absorbing membrane is required.
Horizontal bone augmentation: "staged" approach with an L-PRF bone block

Most steps are similar to those in previous video. The L-PRF bone-block is well adapted to the native bone. Small perforations in the cortical bone guarantee an optimal blood supply and a strong connection between graft and native bone. The slow-absorbing or non-absorbing membrane and membrane tacks provide extra stability to the graft. L-PRF membranes, covering the slow- absorbing membrane, protect the regenerate in case of a wound dehiscence. Primary closure will facilitate the healing.
So far it is not well understood whether a slow- absorbing or non-absorbing membrane is required.
infra bony defect treated with L-PRF as single substitute

The initial steps of periodontal therapy have to be completed first. After preparing a minimally invasive flap, a thorough root planing & removal of all granulation tissue is crucial, rinse socket with L-PRF exudate. The intra-bony defect is filled with chopped L-PRF membrane (preferably face portion) and covered with L-PRF membranes. Ensure the latter extend over the buccal and lingual bony borders. Primary closure should be obtained.
For this indication, several strategies have been proposed, but this protocol seems to be most logical.
If you like to learn more about the use of L-PRF for different surgical applications and/or for wound care, please visit my website.
(open since May 10th, 2025). You can also use this URL: www.l-prf4all.com
Web-Design - Jeroen Van der Putten
Layout & Design - Bianca Thys
With permission: Quirynen M, Pinto N. Leucocyte- and Platelet-Rich fibrin in Oral Regenerative Procedures. Evidence Based Clinical Guidelines. Berlin: Quintessence Publishing 2022.